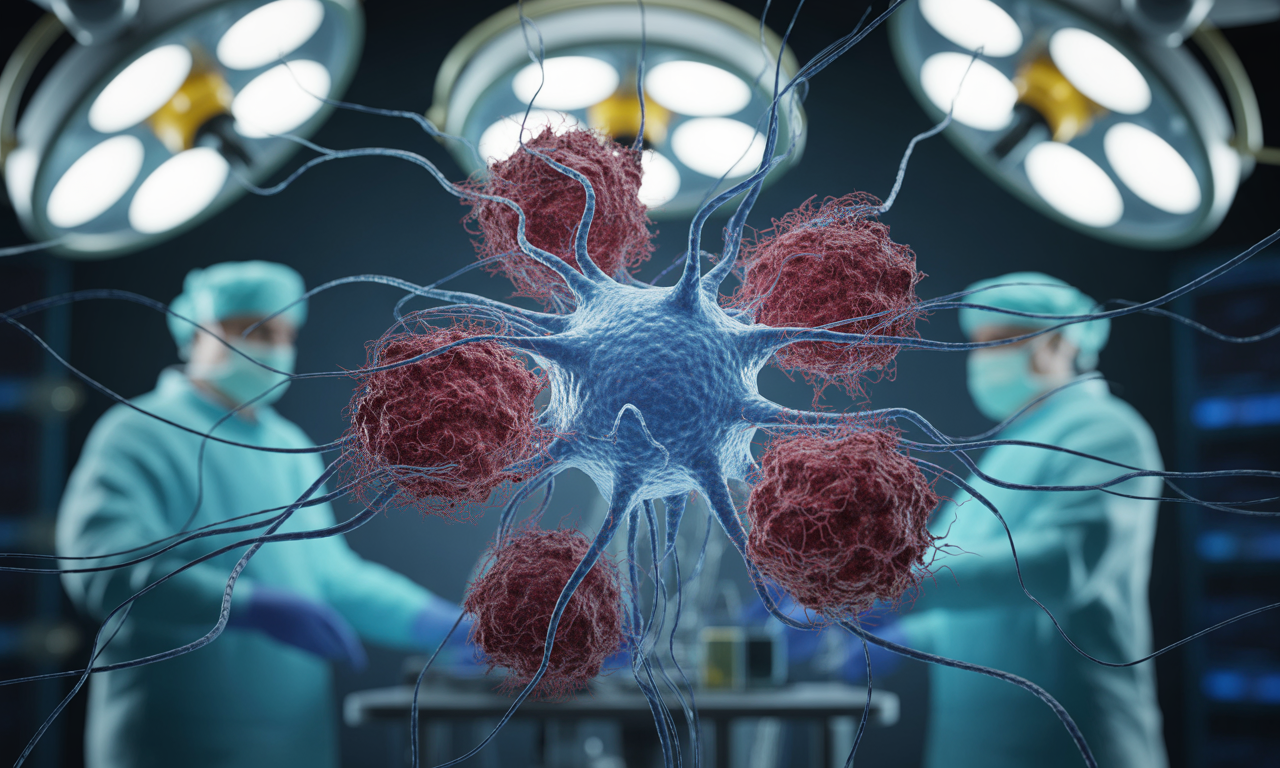
Nature study shows cancer-induced nerve injury drives resistance to anti-PD-1 therapy; IL-6/IFN pathways emerge as actionable targets.
🧠 What’s New
A multi-institutional team led by Moffitt Cancer Center, Karolinska Institutet, and MD Anderson has uncovered a previously unknown mechanism by which cancers co-opt the nervous system to resist immunotherapy. Published today in Nature, the study shows tumors infiltrate and damage nearby nerves, triggering chronic inflammation that ultimately suppresses anti-tumor immunity and diminishes response to anti-PD-1 treatment.
🔬 How Cancer Damages Nerves
- Tumor–nerve interaction: Cancer cells invade tumor-associated nerves and degrade the myelin sheath that insulates nerve fibers.
- Cancer-induced nerve injury (CINI): Myelin loss disrupts electrical conduction and kicks off a nerve-repair program.
- Inflammatory cascade: Damaged neurons release signals that activate interleukin-6 (IL-6) and type I interferons—initially protective, but harmful when the injury persists.
🧯 From Repair to Resistance
- Acute to chronic shift: As tumors continue injuring nerves, the repair response becomes chronic inflammation.
- Immune suppression: The prolonged IL-6/type I IFN signaling remodels the tumor microenvironment into a suppressive state, exhausting immune cells and reducing the effectiveness of anti-PD-1 immunotherapy.
- Clinical correlation: Patients with perineural invasion or CINI exhibit poorer responses to checkpoint inhibitors across multiple tumor types.
🧪 Evidence Across Cancers
The findings were validated using patient samples and models from:
- Cutaneous squamous cell carcinoma
- Melanoma
- Gastric cancer
- Pancreatic cancer
Perineural invasion emerged as a negative predictor for anti-PD-1 response, underscoring the clinical relevance of the nerve–tumor interplay.
💊 Therapeutic Opportunities
The team demonstrated several strategies that partially or fully reversed resistance:
- Surgical denervation: Removing specific pain-transmitting nerves to reduce pro-resistance signaling.
- ATF3 pathway modulation: Conditional knockout of ATF3, a transcription factor linked to neuronal injury responses.
- Interferon-α receptor blockade: Disrupting type I IFN signaling to prevent chronic immune exhaustion.
- Combination therapy: Pairing anti-PD-1 with IL-6 pathway inhibitors to reprogram the inflamed, suppressive tumor microenvironment.
These interventions point to a new class of “neuro-immuno-oncology” combinations that could benefit patients with perineural invasion—a common poor-prognosis feature.
🧭 Why This Matters
- New biology: Defines cancer-induced nerve injury (CINI) as a driver of immune evasion—not just a bystander effect.
- Biomarker potential: Perineural invasion and neural injury signatures may help predict which patients are less likely to benefit from checkpoint inhibitors alone.
- Translational path: Supports clinical trials testing anti-PD-1 plus IL-6 inhibitors or IFN-pathway modulation, and integrating nerve-focused imaging or pathology into treatment planning.
🧓 Patient Impact
- Better selection: Patients with evidence of perineural invasion could be triaged to combination approaches upfront.
- Expanded options: Those who previously failed anti-PD-1 therapy might benefit from IL-6–targeted combinations or pathway-specific inhibitors.
- Quality of life: Addressing tumor–nerve crosstalk may also help manage cancer-associated pain and neurological symptoms.
Frequently Asked Questions❓
- What is cancer-induced nerve injury (CINI)?
A process where tumors invade and damage nerves, degrading myelin and triggering a sustained inflammatory repair response that ultimately suppresses anti-tumor immunity. - How does this cause immunotherapy resistance?
Chronic IL-6 and type I interferon signaling reprograms the tumor microenvironment, exhausting immune cells and blunting anti-PD-1 efficacy. - Which cancers are affected?
Evidence spans cutaneous squamous cell carcinoma, melanoma, gastric, and pancreatic cancers, with broader implications wherever perineural invasion occurs. - Are there treatment options now?
Preclinical strategies include denervation, ATF3 modulation, IFN-α receptor blockade, and combining anti-PD-1 with IL-6 inhibitors—pointing to near-term clinical trial opportunities. - What should clinicians watch for?
Pathology reports indicating perineural invasion; consider multidisciplinary evaluation and trial enrollment for neuro–immune–targeting combinations.
🧩 For Researchers and Marketers
- Messaging: Position perineural invasion as a dual biomarker of poor prognosis and immunotherapy resistance risk.
- Education: Explain the nerve–tumor–immune triad in patient-friendly language, emphasizing actionable next steps (biopsy review for PNI, trial options).
- Pipeline fit: Highlight IL-6 and type I IFN pathway inhibitors as rational partners with anti-PD-1.
🏢 About DNA Labs India
DNA Labs India supports oncology programs with advanced molecular profiling, biomarker education, and content development. For integrating neuro–immune insights into clinical pathways or patient education, connect with our team.